Featured
Rising Stars of Clinical Science
At APS 2022, rising researchers share new insights on stigma, language, reward positivity.

Photo Above: Attendees at the 2022 APS Annual Convention applaud one of dozens of scientific presentations during the event.
The COVID-19 pandemic disrupted the lives and work of countless clinical psychologists, but for researchers like Katie Wang, the impact was especially personal. An assistant professor in the Department of Social and Behavioral Sciences at the Yale School of Public Health, Wang (a 2021 APS Rising Star) is also blind. Her research takes an interdisciplinary look at stigma as a psychosocial determinant of mental and behavioral health inequities among marginalized populations, with a specific emphasis on people with physical disabilities and mental health conditions.
In a forum at the 2022 APS Annual Convention in May, Wang and other “rising stars” of clinical science outlined research that could be shaping future directions in the field. One of her projects is informed by her personal experience as a member of the disability community. It explores the COVID-19 pandemic’s mental health impact on people whose disabilities have exacerbated challenges such as obtaining basic supplies, securing transportation, and being disproportionately exposed to pandemic-related adversities, including social isolation and loss of employment and/or income.
“The faster we can collect this data and get our findings out there, the faster we can start developing interventions to mitigate the impact of COVID-19 on the disability community,” Wang explained in this video recorded in late 2020. In a study of 441 U.S. adults with disabilities, Wang and researchers from several peer institutions sought to identify the demographic and psychosocial predictors of depression and anxiety symptoms in adults with disabilities, as well as to identify subgroups who were particularly vulnerable to the pandemic’s adverse mental health impact.
Learn more about Katie Wang in this Back Page interview.
In an online survey administered from October through December 2020, Wang and colleagues found that 61% of participants met diagnostic criteria for probable major depressive disorder and 50% for generalized anxiety disorder. Participants also showed significantly higher levels of disability-related stigma and social isolation compared to pre-pandemic norms. These and other findings have significant public health implications for how to better support people with disabilities, Wang said. They include the need to expand virtual communities and support groups that connect people with disabilities; educate health care providers about ableism, which can manifest in attitudes and practices that hinder people with disabilities from receiving equitable medical care; and ensure greater use of public health measures to prevent the spread of COVID-19 and other diseases.
Wang also shared preliminary findings from a 5-year study of mental illness stigma as a risk factor for substance use. In future work, she hopes to better understand the intersectionality of disability with other identities, the intertwining experiences of ableism and racism, and barriers to seeking mental health treatment among people with disabilities.
Linguistic processes and cognitive reappraisal
How does language influence our ability to regulate our emotions and manage our mental health? Moreover, can we manipulate language to actually improve emotion regulation and well-being? “I’m fascinated by the idea that psychotherapy is essentially a set of conversations,” said Erik C. Nook in his presentation at the 2022 APS convention. A postdoctoral fellow at Yale University and, as of this fall, an assistant professor of psychology at Princeton University, Nook studies how language and emotion interact, focusing on the development, representation, and regulation of emotion and the clinical implications of these processes.
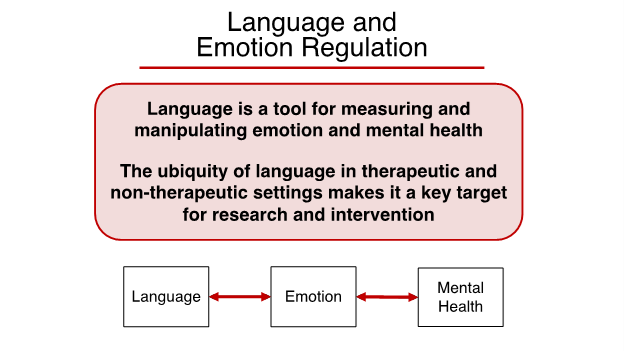
In conversations between patients and therapists, “words are therapeutic instruments as well as a powerful and ubiquitous entry point for mental health,” Nook explained. He presented research exploring how manipulating certain linguistic processes can support cognitive reappraisal, which involves reinterpreting a situation to alter its meaning or impact. When people use cognitive reappraisal, he and colleagues found, they spontaneously distance their language—talking less about themselves and the present moment. People who distance their language more strongly, in turn, are more successful at regulating their emotions. “More distancing reflects better reappraisal,” he said.
In one experiment, Nook asked participants to use several types of linguistic distancing—physical, social, and temporal—to write how they felt after briefly being exposed to images of aversive stimuli such as cockroaches, spiders, accidents, and explosions. Simply by writing about these negative scenes as occurring far away, not using “I” or “me” pronouns, or not using present-tense verbs, participants reported feeling better. “Merely increasing the distance in one’s language can downregulate negative emotion.”
Another study translated this line of basic research into the e-clinic. Analyzing 1.2 million texts from more than 6,200 participants using the Talkspace online therapy platform, Nook found that participants’ internalizing symptoms decreased over time as they shifted their language away from themselves and the present.
Concluding, Nook expressed optimism for using language to measure and manipulate emotion and mental health. “The ubiquity of language in therapeutic and nontherapeutic settings makes it a key target for research and intervention,” he said.
The predictive power of reward positivity
In her presentation, Katie Burkhouse, an assistant professor of psychiatry at Nationwide Children’s Hospital and The Ohio State University, examined the role of neural reward responsivity in the treatment and prevention of depression across development. Major depressive disorder ranks as the fourth leading cause of disability worldwide and is associated with substantial socioeconomic cost in the United States, she noted. But success varies widely even for the “gold-standard” treatments of cognitive behavioral therapy (CBT) and selective serotonin reuptake inhibitors (SSRIs), the most commonly prescribed antidepressants.
Why study reward positivity (RewP), or how individuals respond to rewards or positive feedback? “Because it’s heavily implicated in depression risk,” Burkhouse explained. “It’s more attenuated in youth and adults who have or are at risk of depression.” Many depressive disorders, in fact, are characterized by diminished hedonic responses and an inability to modulate behavior as a function of rewards.
Some of Burkhouse’s research has explored two questions: Can RewP be used to predict how someone will respond to CBT or SSRI treatment, and are gold-standard treatments for MDD effective in enhancing RewP? In two studies—one with 52 adults and one with 27 children and adolescents, all with depression and anxiety—blunted RewP (measured via EEG after participants performed a reward task) did indeed predict greater baseline depressive symptoms. But the researchers found no evidence that CBT or SSRI increased RewP overall, although adults with greater deficits in reward reactivity did perform better with CBT.
Burkhouse also shared research aimed at preventing depression in the children of depressed mothers, who have been shown to be 3 to 4 times more likely to develop MDD than children of nondepressed mothers. One promising group-based program, developed by Bruce Compas at Vanderbilt University, helps mothers cope with depression and improve parenting skills and teaches children coping skills for managing stress within their families and environment. In her presentation, Burkhouse showed that high-risk youth who exhibited a more blunted reward response at baseline, assessed via the RewP, were more likely than those with intact reward-processing styles to respond to the prevention program.
Burkhouse pointed out that in her prior studies, although individual differences in reward reactivity have predicted treatment responses, standard interventions and prevention programs for depression have been generally ineffective in enhancing reward-processing deficits in individuals with depression. Thus, in another ongoing project, Burkhouse and her colleague Autumn Kujawa at Vanderbilt are collaborating on a novel prevention program called Families Promoting Positive Emotions (F-PPE), a prevention program designed to directly enhance positive affect in mothers and their offspring. Over eight sessions, mothers with depression characterized by anhedonia and their children learn a variety of skills to enhance positive affect at the individual and family level. Future investigations will evaluate the efficacy of F-PPE in a larger sample of at-risk youth and evaluate whether F-PPE exerts its effects through targeting reward response across behavioral and brain units of analysis.
Feedback on this article? Email [email protected] or login to comment.





APS regularly opens certain online articles for discussion on our website. Effective February 2021, you must be a logged-in APS member to post comments. By posting a comment, you agree to our Community Guidelines and the display of your profile information, including your name and affiliation. Any opinions, findings, conclusions, or recommendations present in article comments are those of the writers and do not necessarily reflect the views of APS or the article’s author. For more information, please see our Community Guidelines.
Please login with your APS account to comment.