Featured
A Medical Masquerade: COVID-19 and Racial Disparities in Health

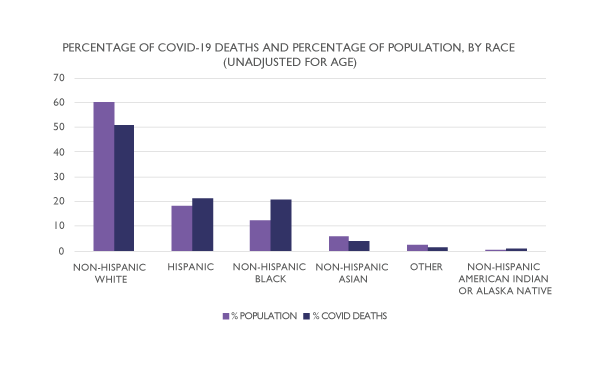
As of October 16, 2020, the novel coronavirus known to cause COVID-19 has infected over 39 million people, contributing to more than 1 million deaths worldwide—but while the effects of this pandemic have been global, they have not been universal. In the United States in particular, the COVID-19 pandemic has had a disproportionate impact on people of color, with Black, Hispanic/Latino, and Native American individuals testing positive for the virus at more than 2.5 times the rate of Whites and being significantly more likely to die from a coronavirus infection, according to the Centers for Disease Control and Prevention (CDC).
Racial differences in illnesses are not the result of biological or even behavioral differences in race but a result of racist, capitalist systems that structure people’s lives.
Whitney N. Laster Pirtle (University of California, Merced)
This heightened risk is nothing new. While COVID-19, as a pandemic, may be classified as a natural disaster, the socioeconomic conditions that have made communities of color disproportionately vulnerable to the virus—including segregation, poverty, and discrimination—are socially constructed, as Sage J. Kim and Wendy Bostwick (University of Illinois) explained in a recent article in Health Education and Behavior. In their analysis of COVID-19 deaths in Chicago, for example, Kim and Bostwick found that cases were clustered on the south and west sides of the city, predominantly African American areas where people were also more likely to have multiple chronic diseases such as asthma and hypertension, which may further increase individuals’ vulnerability to coronavirus.
People of color are also more likely to be employed as essential workers, according to the CDC. This may increase their exposure to COVID-19 through overcrowded conditions in farms and factories, in addition to workplaces such as grocery stores and health care settings that require face-to-face interactions with members of the public, who may or may not wear masks or follow social-distancing recommendations.
“To be clear,” wrote sociologist Whitney N. Laster Pirtle (University of California, Merced) separately in an article published in Health Education and Behavior, “these racial differences in illnesses are not the result of biological or even behavioral differences in race but a result of racist, capitalist systems that structure people’s lives.”
These systems perpetuate unequal access to health care for everyone in the United States through the privatization of insurance—which may make even basic medical care prohibitively expensive to people who are homeless, unemployed, working part-time, or even working full-time for low wages. They are uniquely damaging, however, to people of color living in low-income neighborhoods, Laster Pirtle wrote. People in lower-income areas often have less green space for exercise and are more likely to be near pollutant-producing manufacturing facilities or in “food deserts” where it can be difficult to obtain affordable, healthy meals, she explained. They also tend to receive lower-quality health care—either because of the unequal distribution of resources or because of providers’ racial and economic biases. Combined, these factors also increase individuals’ vulnerability to pre-existing conditions such as obesity, diabetes, and heart disease, which can then exacerbate COVID-19’s effects on the body.
Race as a Process
While there is a consistent pattern of racial disparities in health in the United States, people don’t start out life “Black” or “White,” as APS James McKeen Cattell Fellow James S. Jackson (University of Michigan) explained during his 2012 keynote address at the 24th APS Annual Convention. Instead, individuals become racialized over time.
“The racial group differences that we observe are really only a masquerade,” Jackson said. “As [people] traverse the life course and its stressors—environmental, social, psychological, and economic—those groups actually grow apart.”
Racial health disparities begin to grow in the first year of life, when African American infants are more than twice as likely to die as non-Hispanic White infants.
That growing apart begins in the first year of life, during which African American infants are more than twice as likely to die as non-Hispanic White infants. After this initial loss, however, the physical health disparity generally flips, Jackson explained: From 1999 to 2004, for example, African Americans were less likely to die of endocrine, nutritional, and metabolic diseases in childhood or young adulthood than White youths. This may be partly because infant mortality selects for health, meaning that African American babies who survive the first year of life may be healthier, on average, than White babies who had access to better-quality care.
Health outcomes begin to diverge again, though, as people enter middle age and later life, when stressors, along with coping strategies such as smoking, drinking, and unhealthy eating, begin to take their toll. At this point, Jackson explained, African Americans begin to experience worse physical health outcomes, on average, whereas Whites experience worse mental health outcomes, including higher rates of major depression and anxiety.
These differing outcomes, according to Jackson’s Environmental Affordances (EA) model, reflect the mounting impact of individuals’ social environments, including sources of stress, such as poor-quality housing or experiences of discrimination, and opportunities for stress relief, such as green spaces and liquor stores, which may lead individuals to favor different coping strategies and to respond to those strategies differently.
Jackson and colleagues Katherine M. Knight and Jane A. Rafferty (University of Michigan, Ann Arbor) examined how the EA model interacts with depression in a 2010 article in the American Journal of Public Health. Using data from 2,780 participants who responded to surveys in two waves of the Americans Changing Lives study, the researchers found the relationship between stressful life events and the onset of depression to be weaker in Black participants who engaged in more poor health behaviors, such as smoking, drinking, and overeating, than those who did not. White individuals who engaged in many poor health behaviors, on the other hand, exhibited a stronger relationship between stressful life events and depression than those who abstained.
“Over the life course, ” Jackson and colleagues concluded, “coping strategies that are effective in ‘preserving’ the mental health of Blacks may work in concert with social, economic, and environmental inequalities to produce physical health disparities in middle age and late life. ”
These coping behaviors reflect adaptive responses to the maladaptive environments African Americans are more likely to live in, Jackson explained, allowing individuals to blunt their psychological response to chronic stress at the cost of their long-term physical health. White individuals who engage in these behaviors do not, on average, experience the same benefits to mental health, Jackson continued, because their mental health is typically more protected by their environments to begin with.
“This is not a story about race,” Jackson stressed. “It is a story about the ways in which privilege is conveyed. . . When you unpack that and you look at people regardless of what their race is, when they have not lived those protected kinds of lives, you indeed get the [same] effects.”
During his 2012 keynote address, Jackson used propensity score analysis to demonstrate the connection between privileged environments and health outcomes in order to, in his words, “turn Whites Black.” This allowed him to mask participants’ self-reported race before computing who was more statistically likely to be Black or White given their life circumstances. As expected, participants who had more in common with the average Black participant, regardless of their actual skin tone, were found to use physically unhealthy behaviors to successfully alleviate psychological stress, which correlated with reduced rates of mental disorders and heightened physical health issues. Similarly, participants who had more in common with the average White participant responded to these behaviors with worsening mental health but had better physical health overall, regardless of their actual race.
“This is a clear instance when, indeed, life context masquerades as a racial group difference,” Jackson said.
How Socioeconomic Status—and Stress—Enter the Body
Among the most influential of these life contexts is socioeconomic status (SES), which has been empirically recognized as a primary determinant of health since at least the 1990s, wrote APS James McKeen Cattell Fellow Nancy E. Adler and Alana Conner (University of California, San Francisco) in a 2003 article in Current Directions in Psychological Science. In fact, there is evidence that individuals’ physical and mental health declines as their SES decreases even in countries with universal health care, suggesting this relationship may represent a cumulative effect of reduced access to a range of resources including not only health care but education and income, as well as the knowledge, social networks, and higher-quality housing and nutrition that these advantages afford. Individuals with low SES are also likelier to inhabit environments that expose them to more physical and social risks, such as pollution, noise, overcrowding, and crime.
The Racial Wealth Gap
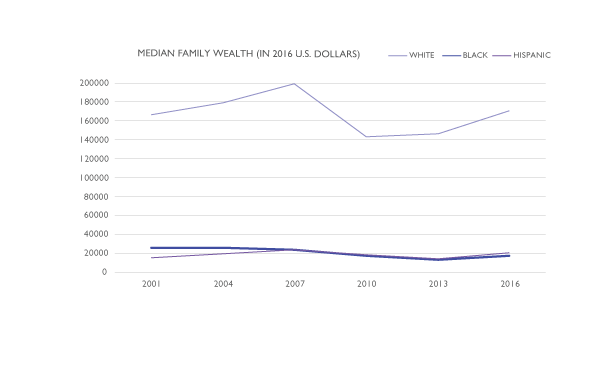
As APS Fellows Michael W. Kraus and Jennifer Richeson (Yale University) and colleagues reported in a 2019 issue of Perspectives on Psychological Science, Americans vastly underestimate the racial wealth gap in the United States. “The magnitude of these misperceptions is substantial,” Richeson and colleagues wrote, “with respondents estimating that for every $100 in wealth held by a White family, a Black family has $90, when, in reality, that Black family has $10.” In 2016, according to the Urban Institute, that difference amounted to a median household wealth, including all assets and debts, of $171,000 for a typical White family and just $17,409 for a typical Black family—a state of massive inequality with serious implications for both physical and mental health.
This relationship exists across the SES spectrum, with the wealthy boasting better health than the middle class, who are in turn healthier than those below the poverty line. But the effect is strongest at lower income levels, Adler and Conner continued, influencing everything from rates of infant mortality to cardiovascular disease, schizophrenia, and substance abuse. A study of British civil servants, for example, found that state employees at the highest pay grade had significantly lower mortality than those who worked lower-paying positions even after they retired.
“As SES decreases, individuals are exposed to more demands and have fewer resources with which to address them,” Adler and Conner wrote. “Biological responses to [this] stress are functional in that they mobilize energy for a ‘fight or flight’ response, but the cumulative effects. . . may increase vulnerability to disease.”
One mechanism through which SES “gets into the body,” Adler explains, is through the dysregulation of multiple physiological systems involved in the stress response over time—a phenomenon known as allostatic load. This “cumulative wear and tear” can increase vulnerability to a range of diseases. Chronic stress can also make individuals more reactive, increasing their sensitivity to stress in the future.
Further, growing up in resource-deprived neighborhoods may increase the prevalence of psychiatric disorders such as depression, anxiety, and attention-deficit/hyperactivity disorder (ADHD) by influencing brain development in areas associated with reward anticipation. In a 2020 study published in Psychological Science, Teagan S. Mullins, Ethan M. Campbell, and Jeremy Hogeveen (University of New Mexico) leveraged existing data from 6,396 American children, 51% of whom were White, who participated in the Adolescent Brain Cognitive Development study. As part of that study, the children were presented with the opportunity to win or lose anywhere between 20 cents and $5 per trial by reacting to stimuli under a time limit while undergoing functional MRI.
Through comparing parents’ responses on a child-behavior checklist as well as the average SES of families living in their zipcode, Mullins and colleagues found that children from low-SES neighborhoods exhibited reduced activity in areas of the brain associated with reward anticipation, which also correlated with increased parent-reported symptoms of psychopathology.
“Impaired reward-motivated behavior and attention problems can have devastating consequences as children progress through adolescence and adulthood,” including increased likelihood of substance abuse and criminal behavior, Mullins and colleagues wrote.
Perceived personal control, particularly in the workplace, also appears to moderate the relationship between SES and health, Adler and Conner explained. They cited a 1998 study by Margie E. Lachman and Suzanne L. Weaver (Brandeis University) in which low-SES people who reported having more control in their personal and professional lives also reported similar rates of depression, chronic health issues, and other health conditions as higher-SES participants.
“Although a substantial portion of the racial-ethnic differences in health is due to social disadvantages associated with low SES, unique effects specific to race-ethnicity also exist, reflecting experiences of discrimination, residential segregation, negative stereotypes, and other circumstances,” Adler and Conner noted.
Discrimination and Health Intersect
Experiences of racial discrimination also play a significant role in the health disparities experienced by African Americans and other people of color in the United States. In a 2017 study led by Lee M. Pachter (Nemours Alfred I. DuPont Hospital for Children) and reported in the Journal of Racial and Ethnic Health Disparities, Jackson and colleagues found that 90% of 1,170 African American and Afro-Caribbean youths surveyed reported experiencing discrimination. And although Jackson has found rates of depression and anxiety to be lower in Black than White individuals generally, discrimination was also linked to higher annual and lifetime rates of depression and anxiety among Black participants.
Racial bias specifically has also been linked to physical health—in particular, to heart conditions such as hypertension—and while researchers must often limit themselves to studying participants’ perceptions of racial bias, one 2016 study published in Psychological Science illustrated a more direct approach. Using racial-bias data generated by over 1 million White participants between 2003 and 2013 as part of Project Implicit, Jordan B. Leitner (University of California, Berkeley) and his colleagues were able to compare Whites’ implicit and explicit racial bias scores with county-level racial disparities in circulatory-disease risk and related deaths.
Racial bias specifically has also been linked to physical health—in particular, to heart conditions such as hypertension.
As part of Project Implicit, led by APS William James Fellow Anthony G. Greenwald (University of Washington) and APS Fellow Brian Nosek (University of Virginia), participants self-reported their feelings of warmth toward European Americans and African Americans, a measure of explicit bias, in addition to completing an Implicit Association Test (IAT). In this case, the IAT required participants to implicitly categorize Black and White faces as either “good” or “bad.” A participant who responded faster when White was paired with “good” and Black was paired with “bad” than when the categories were reversed (Black with “good” and White with “bad”) might be said to hold anti-Black implicit bias. Project Implicit also collected participants’ IP addresses, which allowed Leitner and colleagues to compare individuals’ locations with CDC data collected from over 23,000 Black respondents in 208 counties and 175,000 White respondents in 210 counties in 2012.
In areas where White respondents reported higher levels of explicit racial bias, Black participants were 8% less likely than Whites to report access to affordable health care, compared to 3% less likely in areas with lower explicit bias. Black individuals were also significantly more likely than White individuals to die of circulatory disease in counties with higher explicit bias. In both cases, implicit bias was not found to relate to African Americans’ cardiovascular health.
Racial bias might interact with disease risk and access to care through multiple pathways, including structural discrimination in the health care system and increased stress from interpersonal hostility, which has been shown to increase the risk of circulatory disease over time, explained Leitner and colleagues.
A similar relationship may exist between dominant-group attitudes and health in other minority groups, the researchers noted. People in the lesbian, gay, bisexual, and transgender (LGBT) community, for example, have been found to have shorter life expectancies in areas with higher levels of antigay attitudes. Because of the way identities intersect, wrote Tené T. Lewis and Miriam E. Van Dyke (Emory University) in a 2018 article in Current Directions in Psychological Science, this kind of stress may compound in unique ways for people who experience discrimination not only because of their race but because of other aspects of their identity, such as their age, gender, sexual orientation, or SES.
While SES has been linked to reduced physical and mental health outcomes across racial groups, for example, African Americans with higher SES often report experiencing more discrimination than those in lower-income settings. This may be because higher-SES African Americans are likelier to live and work in more racially integrated communities, exposing them to more discrimination from people of other races, which may also prevent them from receiving the full health benefits of higher SES, Lewis and Van Dyke explained.
“In this respect, designing studies that acknowledge some of the complexity within races might ultimately lead to a better understanding of factors that shape disparities between races,” Lewis and Van Dyke wrote.
References
Adler, N. E., & Snibbe, A. C. (2003). The role of psychosocial processes in explaining the gradient between socioeconomic status and health. Current Directions in Psychological Science, 12(4), 119–123. https://doi.org/10.1111/1467-8721.01245
Centers for Disease Control and Prevention. (2020, October 6). CDC COVID Data Tracker. https://covid.cdc.gov/covid-data-tracker/#cases_totalcases
Centers for Disease Control and Prevention. (2020, September 17). Health disparities: Race and Hispanic origin. Provisional death counts for coronavirus disease 2019 (COVID-19). https://www.cdc.gov/nchs/nvss/vsrr/covid19/health_disparities.htm
Centers for Disease Control and Prevention. (2020, August 18). COVID-19 Hospitalization and Death by Race/Ethnicity. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html
Centers for Disease Control and Prevention. (2020, July 24). Health equity considerations and racial and ethnic minority groups. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html
Centers for Disease Control and Prevention. (2020, September 23). Health Disparities: Race and Hispanic origin. Provisional death counts for coronavirus disease 2019 (COVID-19). https://www.cdc.gov/nchs/nvss/vsrr/covid19/health_disparities.htm
Centers for Disease Control and Prevention. (2020, September 10). Reproductive health: Infant mortality. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/infantmortality.htm
Jackson, J. S., Knight, K. M., & Rafferty, J. A. (2010). Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health, 100(5), 933–939. https://doi.org/10.2105/AJPH.2008.143446
Kim, S. J., & Bostwick, W. (2020). Social vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Education & Behavior, 47(4), 509–513. https://doi.org/10.1177/1090198120929677
Kraus, M. W., Onyeador, I. N., Daumeyer, N. M., Rucker, J. M., & Richeson, J. A. (2019). The misperception of racial economic inequality. Perspectives on Psychological Science, 14(6), 899–921. https://doi.org/10.1177/1745691619863049
Lachman M.E., Weaver S.L. (1998). The sense of control as a moderator of social class differences in health and well-being. Journal of Personality and Social Psychology, 74(3), 763–773. https://doi.org/10.1037/0022-3514.74.3.763
Laster Pirtle, W. N. (2020). Racial capitalism: A fundamental cause of novel coronavirus (COVID-19) pandemic inequities in the United States. Health Education & Behavior, 47(4), 504–508. https://doi.org/10.1177/1090198120922942
Leitner, J. B., Hehman, E., Ayduk, O., & Mendoza-Denton, R. (2016). Blacks’ death rate due to circulatory diseases is positively related to whites’ explicit racial bias: A nationwide investigation using Project Implicit. Psychological Science, 27(10), 1299–1311. https://doi.org/10.1177/0956797616658450
Lewis, T. T., & Van Dyke, M. E. (2018). Discrimination and the health of African Americans: The potential importance of intersectionalities. Current Directions in Psychological Science, 27(3), 176–182. https://doi.org/10.1177/0963721418770442
Mezuk, B., Abdou, C. M., Hudson, D., Kershaw, K. N., Rafferty, J. A., Lee, H., & Jackson, J. S. (2013). “White Box” epidemiology and the social neuroscience of health behaviors: The Environmental Affordances Model. Society and Mental Health, 3(2), 79–95. https://doi.org/10.1177/2156869313480892
Mullins, T. S., Campbell, E. M., & Hogeveen, J. (2020). Neighborhood deprivation shapes motivational-neurocircuit recruitment in children. Psychological Science, 31(7), 881–889. https://doi.org/10.1177/0956797620929299
Pachter, L. M., Caldwell, C. H., Jackson, J. S., & Bernstein, B. A. (2018). Discrimination and mental health in a representative sample of African-American and Afro-Caribbean youth. Journal of Racial and Ethnic Health Disparities, 5(4):831–837. https://doi.org/10.1007/s40615-017-0428-z
Schaeffer, K. (2019). The most common age among whites in U.S. is 58—more than double that of racial and ethnic minorities. Pew Research Center. https://www.pewresearch.org/fact-tank/2019/07/30/most-common-age-among-us-racial-ethnic-groups/
World Health Organization. (2020, October 16). Coronavirus operational update on COVID-19. https://www.who.int/publications/m/item/weekly-update-on-covid-19—16-october-2020
Urban Institute. (2017, October 5). Nine charts about wealth inequality in America (updated). https://apps.urban.org/features/wealth-inequality-charts/





APS regularly opens certain online articles for discussion on our website. Effective February 2021, you must be a logged-in APS member to post comments. By posting a comment, you agree to our Community Guidelines and the display of your profile information, including your name and affiliation. Any opinions, findings, conclusions, or recommendations present in article comments are those of the writers and do not necessarily reflect the views of APS or the article’s author. For more information, please see our Community Guidelines.
Please login with your APS account to comment.