Presidential Column
The “Obesity Epidemic”
Katherine Flegal is perhaps best known for her work in obesity epidemiology. She has led or participated in numerous research projects using national data to track and characterize trends in the prevalence of obesity and being overweight among both adults and children. These analyses serve to inform much of the work on obesity in populations. She was a leader in the research that first identified the increases in obesity in the United States and also in initiating the use of widely accepted international standards for these estimates. Her important analysis, cited by leading experts, showed that the population weight trends were characterized by differential increases at different weight levels, with the heavier segment of the population becoming much heavier, whereas the leaner segment showed little change, thus providing evidence for a gene-environment interaction. She also published several important papers on the effect of changes in smoking prevalence, due both to decreased initiation and to smoking cessation, on population obesity prevalence, showing both that decreased smoking prevalence contributes to increasing prevalence of obesity and that the contribution is minor.
Flegal’s work showed that over 100,000 deaths per year in the U.S. were associated with obesity, and subsequent work showed that these deaths were concentrated among three major causes: cardiovascular disease, diabetes, and a set of selected cancers. These analyses relied on the development of new statistical approaches to the problem of identifying and quantifying the health burden associated with obesity in the population. Further contributions in this area have evaluated the effects of using different anthropometric measures in such studies. She is continuing work on anthropometry and body composition using various measures in the U.S. population.
Another related area where she has made important contributions is the creation and use of growth charts for children. She was a major participant in the revision of the CDC Growth Charts that appeared in 2000; she was also a collaborator in the development of the IOTF (International Obesity Task Force) standards for overweight and obesity among children, and, subsequently, for thinness among children. She has contributed numerous articles concerning the application and use of these data.
Her methodological work on issues of misclassification in epidemiologic studies has been influential and is cited in numerous textbooks. She has additionally been a contributor to numerous important papers involving the health and mortality impact of blood lead levels in the population and the impact of environmental tobacco smoke.
Bartoshuk: How are data on weight collected?
Flegal: The data that we use all come from NHANES, the National Health and Nutrition Examination Survey [http://www.cdc.gov/nchs/nhanes.htm]. This survey is conducted on a nationally representative sample. Participants are first interviewed in the household and then invited to attend a health examination (physical examination) in a special mobile examination center, staffed by technicians and health personnel. The examination includes measures of height and weight as well as numerous other examination components and laboratory measurements. The survey began in 1960 and was conducted on a periodic basis until 1999 when it became a continuous survey. These cross-sectional data provide a snapshot of the U.S. population at successive points in time.
Because we have measured weights and heights on representative samples of the [civilian, non-institutionalized] U.S. population dating back to 1960, we can look at population trends over time. The surveys are cross-sectional, not longitudinal, so we don’t have data on individual changes in weight, but rather data on the population over time. We generally use body mass index (BMI) calculated as weight in kilograms divided by height in meters squared. This index was suggested originally by the Belgian statistician Adolphe Quetelet [1796-1874] and is now very widely used.
Using the current widely accepted definition of obesity as a body mass index [BMI] of 30 or above, we saw that from 1960 through 1980, there was little change in the prevalence of obesity among adults. However between the survey in 1976-1980 and the survey in 1988-1994, the prevalence of obesity increased noticeably by approximately eight percentage points, for reasons that have never been really explained, although speculation is rife [e.g., see Keith et al., 2006; McCrory, Suen & Roberts, 2002; Prentice & Jebb, 1995].
Bartoshuk: Could you describe what the most important features of the weight data are with regard to the obesity epidemic?
Flegal: These increases and subsequent increases have some striking features. First off, the prevalence of obesity in the population generally varies by a number of factors, such as sex, age, race-ethnic group, educational levels and smoking status. The increases in obesity, however, occurred in all these groups fairly uniformly, suggesting that the factors that cause variation in obesity prevalence in the population are not necessarily the same as the factors causing the increases in prevalence. The trends observed for children are similar to those for adults. Similar trends are seen in many developed countries at a similar time.
Plots of the changes of the distribution of BMI show that over time the distribution isn’t moving uniformly to the right, however. The distribution is becoming much more skewed. The lower end of the BMI distribution in the population is pretty similar over time, but the higher end is considerably higher. This suggests some kind of effect that varies by BMI level, possibly a gene-environment interaction, where those who are not genetically susceptible to the effects of the environment are little affected. However, it could also suggest social or personal factors that interact with the environment as well. Some groups may be socially more protected from the effects of the environment, with its ample, cheap food supply and the limited need for physical activity, than other groups.
The prevalence of obesity appeared relatively stable over about a 20 year period from 1960 to 1980, then increased noticeably between 1980 to 1988-1994, then again to 1999-2000 [see Figure 1]. After that point, the increases diminished and obesity prevalence may have restabilized, particularly for women and children, or at least changing at a much slower rate.
Bartoshuk: What do the data say to you?
Flegal: Although these phenomena are often referred to as the obesity “epidemic,” the word may be misleading. An epidemic is a number greater than expected, but what would be the expected prevalence of obesity? The prevalence in 1960, which was about 15 percent? Obesity might more properly be regarded as endemic, not epidemic. Data dating back to the Civil War, though limited, suggests that weight has been increasing fairly steadily ever since and increasing at a slower rate now than it did in the last half of the 19th century. A broader perspective then would suggest that the current trends in obesity are a further manifestation of this longer-term trend and not a sudden outbreak of a disease.
The distribution of BMI is sometimes viewed as though it were a behavioral distribution — as you move from left to right, physical activity decreases and food intake increases. More likely, the distribution, like other roughly normal distributions, is arising from the effect of myriad factors, including individual behavior, genetic make-up, and environmental factors. It is surprising how little we have learned about the factors underlying these trends.
Bartoshuk: How do these data relate to mortality?
Flegal: In our work, we have also addressed issues of the number of deaths in the United States that are associated with different BMI levels. When we look at the most recent mortality data from following the 1988-94 survey through 2000, it suggests that the association of overweight — a BMI from 25-29.9 — and even of mild obesity — BMI 30-34.9 — with mortality is weak and not statistically significant. Although other measurements such as waist circumference are often thought to be better than BMI as indicators of risk, we found no significant differences between BMI and a number of other measures, with BMI actually associated more strongly with mortality than the other measures. One of our findings was that the association of weight and mortality seems to be much weaker in the more recent data, leading us to the suggestion that perhaps the association is diminishing over time, perhaps because of improvements in public health and in medical care, a suggestion that has proved to be somewhat surprisingly controversial [e.g., see Adams et al., 2006; Calle, Teras, & Thun, 2005; Manson, et al., 2007].
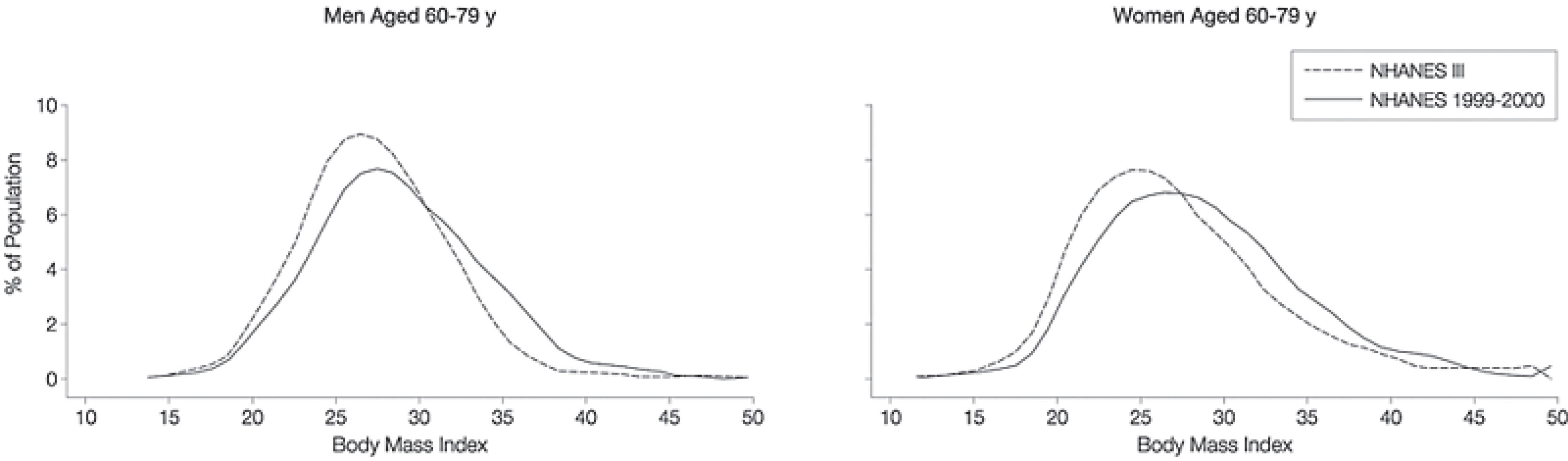 Figure 1: Distributions of Body Mass Index from NHANES III (1988-1994) and NHANES 1999-2000 (Flegal, K.M., Carroll, M.D., Ogden, C.L., & Johnson, C.L. (2002)).
Figure 1: Distributions of Body Mass Index from NHANES III (1988-1994) and NHANES 1999-2000 (Flegal, K.M., Carroll, M.D., Ogden, C.L., & Johnson, C.L. (2002)).
References
Adams, K.F., Schatzkin, A., Harris, T.B., Kipnis, V., Mouw, T., Ballard-Barbash, R., et al. (2006). Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. New England Journal of Medicine, 355, 763-778.
Calle, E.E., Teras, L.R., & Thun, M.J. (2005). Obesity and mortality. The New England Journal of Medicine, 353, 2197-2199.
Cole, T.J., Flegal, K.M., Nicholls, D., & Jackson, A.A. (2007). Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ, 335, 166-167.
Flegal, K.M. (2007). The effects of changes in smoking prevalence on obesity prevalence in the United States. American Journal of Public Health, 97, 1510-1514.
Flegal, K.M., Carroll, M.D., Kuczmarski, R.J., & Johnson, C. L. (1998). Overweight and obesity in the United States: Prevalence and trends, 1960-1994. International Journal of Obesity, 22, 39-47.
Flegal, K.M., Carroll, M.D., Ogden, C.L., & Johnson, C.L. (2002). Prevalence and trends in obesity among U.S. adults, 1999-2000. JAMA, 14, 1723-1727.
Flegal, K.M., & Graubard, B.I. (2009). Estiimates of excess deaths associated with body mass index and other anthropometric variables. American Journal of Clinical Nutrition, 89, 1213-1121.
Flegal, K.M., Graubard, B.I., Williamson, D.F., & Gail, M. H. (2005). Excess deaths associated with underweight, overweight, and obesity. JAMA, 293, 1861-1867.
Flegal, K.M., Graubard, B.I., Williamson, D.F., & Gail, M. H. (2009). Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA, 298, 2028-2037.
Flegal, K.M., & Troiano, R.P. (2000). Changes in the distribution of body mass index of adults and children in the U.S. population. International Journal of Obesity, 24, 807-818.
Keith, S.W., Redden, D.T., Katzmarzyk, P.T., Boggiano, M. M., Hanlon, E.C., Benca, R.M., et al. (2006). Putative contributors to the secular increase in obesity: exploring the roads less traveled. International Journal of Obesity, 30, 1585-1594.
Manson, J.E., Bassuk, S.S., Hu, F.B., Stampfer, M.J., Colditz, G.A., & Willett, W.C. (2007). Estimating the number of deaths due to obesity: Can the divergent findings be reconciled? Journal of Women’s Health, 16, 168-176.
McCrory, M.A., Suen, V.M.M., & Roberts, S.B. (2002). Biobehavioral influences on energy intake and adult weight gain. Journal of Nutrition, 132, 3830S-3834S.
Prentice, A.M., & Jebb, S.A. (1995). Obesity in Britain: Gluttony or sloth? BMJ, 311, 437-439.


APS regularly opens certain online articles for discussion on our website. Effective February 2021, you must be a logged-in APS member to post comments. By posting a comment, you agree to our Community Guidelines and the display of your profile information, including your name and affiliation. Any opinions, findings, conclusions, or recommendations present in article comments are those of the writers and do not necessarily reflect the views of APS or the article’s author. For more information, please see our Community Guidelines.
Please login with your APS account to comment.