Featured
Dueling Diagnoses
Concerns about overlapping symptoms, complex disorders lend momentum to diagnostic models that could supplement—or even supplant—the DSM.

The Diagnostic and Statistical Manual of Mental Disorders (DSM) is so widely used and fundamental to psychiatry and clinical psychology that it is commonly called the “bible” of the mental health profession. Not only does it define disorders and describe their core symptoms and typical course, but it describes why they are included as diagnoses at all, lists indications that a person does not have a disorder, and emphasizes variations in symptoms by age, gender, and culture. And since its initial publication in 1951, the manual has been continually revised to accommodate new scientific insights.
However, despite its increasing status and ongoing refinements, the DSM has never been free of criticism. By the time the fifth and latest edition, known as the DSM-5, was published in 2013, that criticism had reached a fever pitch.
Related content from this issue: National Academies Release Consensus Report on Ontologies in Behavioral Science
One chief complaint about the DSM is that many of its diagnostic categories lack empirical support. “Most of them were formulated decades ago,” Christopher Conway (Fordham University) and colleagues explained in a 2021 Current Directions in Psychological Science article, “when standards of evidence were very different.” Despite continual revisions, for example, the reliability of DSM diagnoses (i.e., consistent agreement between clinicians) has remained low—in fact, as tests for the diagnoses’ reliability improved, their performance worsened (Cooper, 2014).
Other criticisms concern high rates of comorbidity, or overlap, among diagnoses. “Many people… get five [DSM] diagnoses,” said former National Institute of Mental Health (NIMH) director Steven Hyman (Belluck & Carey, 2013). “But they don’t have five diseases—they have one underlying condition.” It’s actually rare, Conway and colleagues noted, for people to fit only one DSM category.
A further complaint concerns heterogeneity within DSM diagnoses. To qualify for a diagnosis, all patients must have a certain number of symptoms—but those symptoms may differ dramatically. For example, according to Isaac Galatzer-Levy (New York University School of Medicine) and Richard Bryant (University of New South Wales, Kensington), there are 636,120 symptom combinations that meet the DSM-5’s criteria for post-traumatic stress disorder (PTSD). Even if certain symptoms are more or less common, this variability raises questions about how likely researchers are to identify a treatment that applies to all, or even most, cases.
These problems are relevant not only for treatment but for research. Valuable information about the variety and severity of symptoms may be lost when researchers collapse them into unitary DSM diagnoses or exclude participants without a requisite number of symptoms (Forbes et al., 2021). To illustrate that point, Conway and colleagues described an imaginary study based on the DSM’s definition of antisocial personality disorder, which would exclude participants whose “only” symptoms were deceitfulness and a lack of empathy. Surely, the authors argued, those two symptoms alone have a major impact on behavior.
Amid these criticisms, what are the alternatives to the DSM? What new avenues and insights do they open up, and what are their chances of supplanting the “bible” of psychiatry?
Enter RDoC
Mere weeks before its publication, one of the most high-profile blows to the DSM-5 came from Thomas Insel, then director of NIMH. In a blog post, Insel proclaimed that the institute would be “re-orienting its research away from DSM categories.” The DSM’s definitions, he noted, were based on experts’ interpretations of presenting symptoms, not objective data. “Symptoms alone rarely indicate the best choice of treatment,” Insel wrote. “Patients with mental disorders deserve better.”
As an alternative, Insel and others at NIMH proposed a new initiative: the Research Domain Criteria (RDoC) project. Its proponents hoped that by giving grant-seeking researchers a new way to classify and structure their research, RDoC would lay the foundation for a new diagnostic system and, ultimately, better mental health treatment.
Learn more: RDOC at 10: Sharpening the Science of Mental Health
RDoC distinguishes six “transdiagnostic” domains, which play a role in the onset or maintenance of multiple disorders: negative valence systems (which respond to aversive contexts), positive valence systems (which respond to rewarding contexts), cognitive systems, social processes, arousal and regulatory systems, and sensorimotor systems. Each domain can be investigated across eight units of analysis. Three of those—behavior, self-report, and “paradigms,” or assessment instruments—are relatively traditional measures. The others, however, reflect more recent approaches to psychopathology: genes, molecules, cells, (neural) circuits, and physiology.
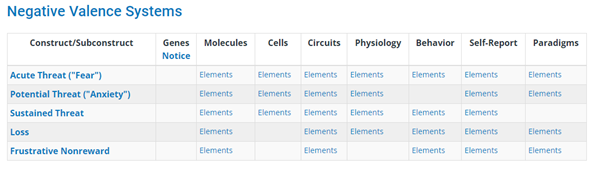

Elements of the National Institute of Mental Health’s Research Domain Criteria (RDoC) matrix. The domain of negative valence systems includes dimensions underlying the ability to respond to aversive or threatening stimuli. The neural circuits governing that domain represent one unit of analysis. Adapted from National Institute of Mental Health, “RDoC Matrix,” https://www.nimh.nih.gov/research/research-funded-by-nimh/rdoc/constructs/rdoc-matrix.
RDoC is thus well positioned to advance understanding of neurobiological processes in psychopathology. For example, as Randy Auerbach (Columbia University) noted in a 2022 article in the Journal of Child Psychology and Psychiatry, although typically developing youth and those diagnosed with attention-deficit/hyperactivity disorder (ADHD) achieve similar cortical maturation over time, that maturation is delayed among ADHD patients. A focus on neurodevelopmental trajectories could help to reveal whether and how this delay relates to behavioral and attentional symptoms. It might even be possible, he proposed, to triangulate across measures—examining how changes in physical development or in hormone levels relate to cortical development and function—to explore how these processes unfold over the course of puberty.
However, because RDoC represents such a sweeping departure from the DSM, it may take a long time for any insights it generates to transform diagnostic models. Insel himself admitted that RDoC might seem to be “divorced from clinical practice”; traditional measures of mental illness may hold their own benefits. “Clinical signs can be poorly specific and/or sensitive markers of diseases,” wrote philosophers of medicine Kathryn Tabb (Bard College) and Maël Lemoine (University of Bordeaux) in 2021. “But at the same time, clinical outcomes are the only variable patients and health practitioners are ultimately interested in.”
Sidebar: Exploring Depression Research Through the Years
In a 2006 article in the Journal of the History of Medicine and Allied Sciences, Laura Hirshbein (University of Michigan) examined how changes in researchers’ theories and practices from the 1950s through the 1980s affected understandings of depression.
In the 1950s, physicians began testing the effects of newly introduced psychiatric drugs. In early trials, researchers administered medication indiscriminately to psychiatric patients and loosely assessed them all for improvements. Calls for greater rigor pushed researchers to define which symptoms to measure, standardize their measurement, and exclude participants with additional conditions.
These practices made for more rigorous science, but they also had unintended effects. Individuals reporting alcohol or substance abuse were excluded from studies of depression, which dramatically reduced the number of male participants. And because samples were often drawn from psychiatric hospitals, whose patients were mostly women, the number of men was cut further.
Moreover, drugs were initially labeled as “antidepressants” if they relieved patients’ depressive symptoms (e.g., by inducing euphoria). But a feedback loop developed, such that relief was taken to confirm a diagnosis of depression, and remediable symptoms became more central to depression scales.
Taken together, Hirshbein argued, these developments colored psychiatrists’ views of depression. Disruptions in emotions and relationships were prioritized; substance abuse and somatic symptoms were not. (Today, those other symptoms’ frequent occurrence in depression is well recognized; see, e.g., Lieb et al., 2007; Nunes & Rounsaville, 2006.)
Hirshbein’s case study illustrates some pitfalls highlighted by Carolyn Wilshire (Victoria University of Wellington) and colleagues in a 2021 article in Clinical Psychological Science. “To understand what symptoms can—and cannot—tell us about mental disorders,” the authors argued, “one must first examine the assumptions that are made about these constructs under different approaches.” Those assumptions include the following:
- Are symptoms reported by individuals or assessed by clinicians, and how much are they shaped by the methods of assessment or individuals’ beliefs?
- Do we see symptoms as fixed entities or as inseparable from theoretical, social, or cultural frameworks?
- How important are descriptions of symptoms’ features, and what methods should we use to develop them?
- How do we view the causal relations among symptoms and between symptoms and mental illness more generally?
- What role do symptoms play in our understanding of mental illness?
Researchers’ answers to these questions—often unstated—shape their investigations, their findings, and their interpretations. Therefore, the authors wrote, creating or refining diagnostic schemes requires us to go further, questioning our approaches to symptoms themselves.
References
Hirshbein, L. D. (2006). Science, gender, and the emergence of depression in American psychiatry, 1952–1980. Journal of the History of Medicine and Allied Sciences, 61(2), 187–216. https://doi.org/10.1093/jhmas/jrj037
Lieb, R., Meinlschmidt, G., & Araya, R. (2007). Epidemiology of the association between somatoform disorders and anxiety and depressive disorders: An update. Psychosomatic Medicine, 69(9), 860–862. https://doi.org/10.1097/PSY.0b013e31815b0103
Nunes, E. V., & Rounsaville, B. J. (2006). Comorbidity of substance use with depression and other mental disorders: From Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) to DSM-V. Addiction, 101(1), 89–96. https://doi-org.proxy.lib.duke.edu/10.1111/j.1360-0443.2006.01585.x
Wilshiren, C. E., Ward, T., & Clack, S. (2021). Symptom descriptions in psychopathology: How well are they working for us? Clinical Psychological Science, 9(3), 323–339. https://doi.org/10.1177/2167702620969215
Network analysis
Network analysis hews more closely to the DSM’s diagnostic categories, retaining the manual’s focus on symptoms but emphasizing their interrelationships, rather than their biological underpinnings. It envisions psychopathology as a network of symptoms and the associations between them. An episode of disorder is thought to occur whenever a sufficient number of associated symptoms arise and persist for long enough to disrupt well-being or functioning. Recovery occurs when symptoms ease or their connections are severed.
In a 2016 article in Behaviour Research and Therapy, APS Fellow Richard McNally (Harvard University) explained that whereas categorical frameworks like the DSM assume that co-occurring symptoms reflect discrete underlying disorders, network analysis assumes that symptoms themselves give rise to disorders and may not share a common cause.
Network analysis also avoids favoring symptoms that are characteristic of or specific to particular disorders. Instead, it emphasizes “central” nodes—the symptoms of greatest importance in a particular network, as evidenced by the number and strength of their associations with other symptoms.
In 2016, APS Fellow Eiko Fried (now at Leiden University) and colleagues reanalyzed data from 3,463 depressed patients who had completed the 28-item Inventory for Depressive Symptomatology (IDS). The IDS assesses many symptoms not found in the DSM, including irritability, anxiety, and somatic complaints (e.g., pain, heavy limbs). The researchers investigated how likely people with one depression symptom were to have other symptoms as well. In a group of people with any condition—such as the measles, Fried suggested in an exchange with the Observer—intercorrelations among disease-specific symptoms (fever, rash) should be higher than intercorrelations among nonspecific symptoms (brittle toenails, dental pain). The researchers’ findings, however, indicated that non-DSM symptoms were just as intercorrelated—that is, as central—as those in the DSM. In other words, a definition of depression could very reasonably include symptoms that the DSM leaves out.
Even if central symptoms apply to a small proportion of sufferers or span many diagnoses, they may hold the key to the emergence—and treatment—of a disorder, according to some proponents of network analysis, because simply unseating a central symptom could help to deactivate other symptoms in the network.
For example, McNally and colleagues found that difficulty sleeping, which isn’t thought to be a core PTSD symptom, was nevertheless a central symptom among survivors of the 2008 Sichuan earthquake. Their results suggested that poor sleep sapped the survivors’ executive resources, hobbling their ability to regulate emotions and attention. If that interpretation is correct, the authors argued, then stabilizing sleep in PTSD patients might be a simple way to bolster the effects of therapy.
Personality traits
But what if symptoms are more than nodes in a network—what if they really dorepresent a latent, underlying factor? When it comes to personality disorders, what we think of as symptoms may simply be “extreme variants of general personality traits,” Thomas Widiger (University of Kentucky) and coauthors wrote in Clinical Psychological Science in 2019. These traits are usually conceptualized as extraversion, neuroticism, openness to experience, agreeableness, and conscientiousness—the dimensions of the five-factor model of personality.
A broad body of research has linked those traits to a variety of meaningful outcomes, including mortality, criminality, school and work performance, life satisfaction, and, of course, psychopathology. For example, Widiger and colleagues noted, evidence from several studies suggests that low conscientiousness and low agreeableness are associated with externalizing psychopathology, which manifests as poorly controlled, impulsive, or aggressive behavior—as seen in substance-use disorders, ADHD, and antisocial personality disorder.
In a 2021 study published in Clinical Psychological Science, Monika Waszczuk (Rosalind Franklin University of Medicine and Science) and coauthors analyzed longitudinal data from three samples—of adolescents, trauma-exposed primary care patients, and psychiatric patients, respectively—to determine whether personality traits predicted the onset of psychiatric disorders, the persistence of symptoms, or functional impairment. Their results indicated that on all three counts, personality traits, especially agreeableness and extraversion, provided more insight than past psychiatric diagnoses.
Both sets of authors concluded that by incorporating personality traits into assessments of patients, clinicians could improve their prognoses and better tailor their treatments. Going one step further, they suggested, mental health interventions might be more successful if they targeted personality traits rather than psychopathy per se.
Personality is often thought to be stable, Widiger and colleagues explained, but in fact it regularly changes, both over the life course and in response to events, including clinical interventions. A mindfulness-based intervention known as the Unified Protocol, for example, was originally developed for mood and anxiety disorders but has since been shown to effectively reduce neuroticism (Barlow et al., 2014).
The authors suggested that it may also be possible to develop interventions to heighten agreeableness and to reduce extreme levels of introversion and openness. In each case, targeting traits, rather than symptoms, might prevent associated manifestations of psychopathology.
But that hope raises questions about causality: Do personality traits cause symptoms or syndromes, Waszczuk and coauthors asked, or do they merely reflect a general underlying vulnerability? Other research is needed, the authors acknowledged, to tease apart those pathways.
HiTOP
One other alternative framework brings together several of these approaches: the Hierarchical Taxonomy of Psychopathology, or HiTOP for short. Drawing on a broad body of empirical work, HiTOP’s proponents argue that all mental illness shares a “general factor” of psychopathology, known as the p factor. That shared general factor, they say, helps to explain the common co-occurrence of symptoms and syndromes.
HiTOP seats the p factor at the top of a hierarchical structure of psychopathology. Directly beneath it are five broad “spectrum constructs”: internalizing, antagonistic externalizing, disinhibited externalizing, detachment, thought disorder, and somatoform. Those constructs are made up of subfactors and, in turn, clusters of symptoms. For example, the internalizing spectrum contains the subfactor of distress, which encompasses key symptoms associated with major depressive disorder (MDD), generalized anxiety disorder, and PTSD. Finally, at the base of the hierarchy are maladaptive personality traits and symptom components.
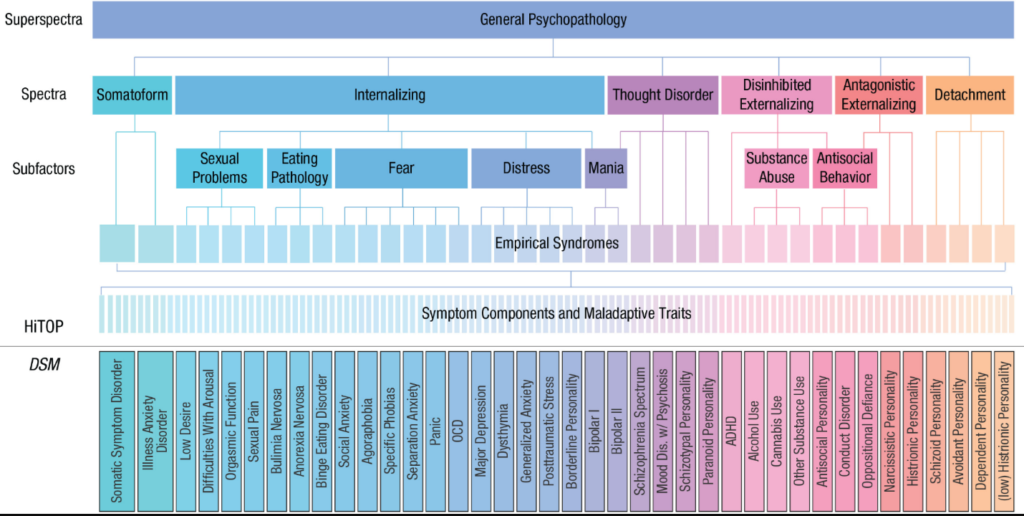
Proponents of HiTOP argue that by collapsing these dimensions, the DSM obscures how symptoms relate to one another and which symptoms are uniquely associated with particular traits and behaviors (Forbes et al., 2021). For example, research into pathological exercise, a common symptom in eating disorders, has found that different motivations underlie this habit among different populations—suggesting that treatments may need to be tailored for overexercisers driven by body-image concerns and by needs for competence and autonomy (Dreier et al., 2020).
Other research influenced by HiTOP has highlighted the dangers of artificially assigning superordinate dimensions of pathology to individual disorders. In a 2020 article in Clinical Psychological Science, Kasey Stanton (University of Wyoming) described recent pushes to recognize negative affective dysfunction (NAD)—characterized by negative moods and maladaptive responses—as a core feature of ADHD. Studies have shown evidence for a substantial association between ADHD and NAD, he acknowledged, so targeting NAD in treatment would obviously be beneficial for some ADHD patients.
However, he wrote, additional evidence suggests that NAD generalizes across internalizing and externalizing disorders and that its association with ADHD is comparatively small. By extension, if the DSM needs to include NAD in ADHD’s diagnostic criteria, then it should also add NAD to the criteria for many other diagnoses.
But doing so would likely increase symptom overlap between ADHD and other disorders, Stanton stressed, with troubling implications for diagnosis and treatment. For example, both MDD and ADHD, as defined by the DSM-5, involve restlessness and difficulty concentrating. If the two disorders also shared NAD as a core symptom, that would make it even harder for clinicians to determine the correct diagnosis for patients—raising the risk of mistaken diagnosis and inappropriate stimulant prescriptions.
ICD
The DSM is sometimes overshadowed by the International Classification of Diseases, or ICD. Since its sixth edition was published in 1949, World Health Organization member states have used the ICD’s categories to report statistics on both mental and physical health. And today, many countries, including the United States, legally require health care professionals to use ICD categories (or national modifications) when collecting or reporting diagnostic information.
It’s no accident that the DSM’s categories are much like the ICD’s: Throughout its history, the DSM has been heavily influenced by the ICD, and that influence has only grown over time. As APS Fellow Lee Anna Clark (University of Notre Dame) and colleagues described in a 2017 article in Psychological Science in the Public Interest, the American Psychiatric Association’s development of the DSM-5 involved collaborations with WHO in “an effort to maximize the [two systems’] structural similarity.” Most criticisms of the DSM also apply to the ICD (Clark et al., 2017), but the ICD’s categorical structure has been less hotly contested than the DSM’s—perhaps because of its underlying goals.
One of those goals is clinical utility—in particular, ease of implementation by relevant health professionals. Moreover, because the ICD is meant to be globally applicable, it has spawned a proliferation of guidelines catering to different needs and populations.
For example, in 1992, WHO developed the ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines (CDDG) to help clinicians make more reliable diagnoses of mental health disorders. Rather than requiring precise symptom durations and counts like the DSM, the CDDG offers more flexible guidance. That flexibility allows not only for cultural variation in presentations of illness but for geographic variation in infrastructure and available resources (Clark et al., 2017).
Another WHO publication, the mhGAP Intervention Guide for Mental, Neurological, and Substance Use Disorders in Non-Specialized Health Settings, details treatment guidelines for primary-care settings in low- and middle-income countries. Limited to “priority” mental disorders—those with the highest prevalence, disease burden, and amenability to treatment—it provides guidance on a range of conditions (including depression, psychoses, dementia, and substance-use disorders), as well as psychosocial interventions (Clark et al., 2017).
Even beyond its clinical use, the ICD has some unique advantages for research. By including mental disorders alongside other medical diagnoses, Clark and colleagues noted, the ICD “facilitates coordination with classification of other disorders, including… conditions that are frequently comorbid with mental and behavioral disorders.” That can also make it easier to identify associations between mental illness and risk factors for other conditions—whether those are due to shared etiology, to patients’ behaviors (e.g., smoking), or to treatment itself (e.g., institutionalization or medication).
Conclusion
Although the DSM’s present-versus-absent symptom and syndrome determinations have been maligned by the proponents of most alternative models, a broad cross-section of users may favor them, as Gerald Haeffel (University of Notre Dame) and colleagues noted in a 2021 Clinical Psychological Science article. In health care and administrative contexts, they explained, binary decisions are often necessary: Does a child qualify for special education? Does an applicant qualify for disability benefits? Can a code be provided to secure insurance coverage for a patient’s treatment? In other words, the same clinical utility that bolsters the status of the ICD makes the DSM valuable, imperfections aside.
The DSM’s monopoly on diagnostic practice might also be weaker than it seems. A recent global survey revealed that mental health professionals found the classifications in the DSM and the ICD most useful for “meeting administrative requirements, assigning a diagnosis, communicating with other health care professionals, and teaching trainees or students, and lowest for selecting a treatment and assessing probable prognosis” (First et al., 2018). In other words, even if clinicians apply DSM categories for administrative purposes, they may incorporate other information into their assessments and treatment decisions.
All of these taxonomic systems have proved useful for certain purposes; improving our understanding and treatment of psychopathology may hinge not on identifying a single system to rule them all but on avoiding what Fried (2021) has called “diagnostic literalism,” or conflating complex mental health problems with cut-and-dry diagnostic categories. In the complex landscape of psychopathology, he cautions, taxonomic systems are useful frameworks for describing the world, reflecting our methods and our needs as much as they reflect reality itself.
Feedback on this article? Email apsobserver@psychologicalscience.org or login to comment.
References
Auerbach, R. P. (2022). RDoC and the developmental origins of psychiatric disorders: How did we get here and where are we going? The Journal of Child Psychology and Psychiatry, 63(4), 377–380. https://doi.org/10.1111/jcpp.13582
https://doi.org/10.1177/2167702613505532
Barlow, D. H., Sauer-Zavala, S., Carl, J. R., Bullis, J. R., & Ellard, K. K. (2014). The nature, diagnosis, and treatment of neuroticism: Back to the future. Clinical Psychological Science, 2(3), 344–365. https://doi.org/10.1177/2167702613505532
Belluck, P., & Carey, B. (2013, May 6). Psychiatry’s guide is out of touch with science, experts say. The New York Times. https://www.nytimes.com/2013/05/07/health/psychiatrys-new-guide-falls-short-experts-say.html
Clark, L. A., Cuthbert, B., Lewis-Fernández, R., Narrow, W. E., & Reed, G. M. (2017). Three approaches to understanding and classifying mental disorder: ICD-11, DSM-5, and the National Institute of Mental Health’s Research Domain Criteria (RDoC). Psychological Science in the Public Interest, 18(2) 72–145. https://doi.org/10.1177/1529100617727266
Conway, C. C., Krueger, R. F., & HiTOP Consortium Executive Board. (2021). Rethinking the diagnosis of mental disorders: Data-driven psychological dimensions, not categories, as a framework for mental-health research, treatment, and training. Current Directions in Psychological Science, 30(2), 151–158. https://doi.org/10.1177/0963721421990353
Cooper, R. (2014, September 2). How reliable is the DSM-5? Mad in America. https://www.madinamerica.com/2014/09/how-reliable-is-the-dsm-5/
Dreier, M. J., Coniglio, K., & Selby, E. A. (2021). Mapping features of pathological exercise using hierarchical-dimensional modeling. International Journal of Eating Disorders, 54(3), 422–432. https://doi.org/10.1002/eat.23406
First, M. B., Rebello, T. J., Keeley, J. W., Bhargava, R., Dai, Y., Kulygina, M., Matsumoto, C., Robles, R., Stona, A.-C., & Reed, G. M. (2018). Do mental health professionals use diagnostic classifications the way we think they do? A global survey. World Psychiatry, 17(2), 187–195. https://doi.org/10.1002/wps.20525
Forbes, M. K., Sunderland, M., Rapee, R. M., Batterham, P. J., Calear, A. L., Carragher, N., Ruggero, C., Zimmerman, M., Baillie, A. J., Lynch, S. J., Mewton, L., Slade, T., & Krueger, R. F. (2021). A detailed hierarchical model of psychopathology: From individual symptoms up to the general factor of psychopathology. Clinical Psychological Science, 9(2), 139–168. https://doi.org/10.1177/2167702620954799
Fried, E. I. (2021). Studying mental health problems as systems, not syndromes. PsyArXiv. https://doi.org/10.31234/osf.io/k4mhv
Fried, E. I., Epskamp, S., Nesse, R. M., Tuerlinckx, F., & Borsboom, D. (2016). What are ‘good’ depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. Journal of Affective Disorders, 189, 314–320. https://doi.org/10.1016/j.jad.2015.09.005
Haeffel, G. J., Jeronimus, B. F., Kaiser, B. N., Weaver, L. J., Soyster, P. D., Fisher, A. J., Vargas, I., Goodson, J. T., & Lu, W. (2022). Folk classification and factor rotations: Whales, sharks, and the problems with the Hierarchical Taxonomy of Psychopathology (HiTOP). Clinical Psychological Science, 10(2), 259–278. https://doi-org.proxy.lib.duke.edu/10.1177/21677026211002500
McNally, R. J. (2016). Can network analysis transform psychopathology? Behaviour Research and Therapy, 86, 95–104. https://doi.org/10.1016/j.brat.2016.06.006
McNally, R. J., Robinaugh, D. J., Wu, G. W. Y., Wang, L., Deserno, M. K., & Borsboom, D. (2015). Mental disorders as causal systems: A network approach to posttraumatic stress disorder. Clinical Psychological Science, 3(6), 836–849. https://doi-org.proxy.lib.duke.edu/10.1177/2167702614553230
Stanton, K. (2020). Increasing diagnostic emphasis on negative affective dysfunction: Potentially negative consequences for psychiatric classification and diagnosis. Clinical Psychological Science, 8(3), 584–589. https://doi.org/10.1177/2167702620906147





Comments
Central Michigan University
Lifetime Member
Member Since 11/20/1992
Terrific article, thanks!
APS regularly opens certain online articles for discussion on our website. Effective February 2021, you must be a logged-in APS member to post comments. By posting a comment, you agree to our Community Guidelines and the display of your profile information, including your name and affiliation. Any opinions, findings, conclusions, or recommendations present in article comments are those of the writers and do not necessarily reflect the views of APS or the article’s author. For more information, please see our Community Guidelines.
Please login with your APS account to comment.